The last two years in healthcare have brought on challenges our industry has never experienced with the onset of COVID-19. As 2022 approaches we begin preparing for post-pandemic operations and take a look at trends in healthcare’s Accounts Payable (AP) departments.
5 AP Trends in Healthcare
Disbursed Workforce
The pandemic has brought on the need for remote workers throughout operations in health systems. Many healthcare organizations plan to keep the remote working structure in place to save on operating and real estate costs.
According to Gartner, 82% of company leaders plan to allow employees to work remotely at least part of the time after the pandemic. Forty-seven percent of company leaders will allow employees to work from home full-time.
However, this new remote work model poses a challenge to our industry’s AP departments. In order to meet new demands, AP leaders must streamline processes that used to heavily rely on manual processing.
To be successful for the long haul, AP Leaders must take action to replace outdated processes and adopt new technology including:
- Digital tools available from any device (laptops, tablets, smartphones)
- Workflow systems that capture important and hard-to-measure data points
- Cloud security and data warehousing
- Collaboration tools such as Microsoft Teams or Skype
- Proper ERP controls and thorough training of the system
As they move to a work-from-home (WFH) model becomes permanent, new communication and collaboration skills are needed as well as additional ways of developing leadership skills within an organization to ensure employees are connected, engaged, and motivated.
Due to many of the issues that the pandemic has created, such as layoffs, staffing shortages, and working with new vendors, AP departments need to rethink workflows. It is now more difficult to determine the appropriate approvers, resolve exceptions, and source the correct information. These issues have staff reporting much longer workdays since the onset of the pandemic.
According to the Institute of Finance & Management (IOFM), 84% of the typical AP FTE’s time is wasted through manual activities.
In order to counteract these challenges, AP must adopt automation tools to process an increased invoice volume.
Examples of Automation AP can utilize:
- Electronic data interchange (EDI) for invoicing
- OCR/Imaging software
- Automated approval workflow
- Payment optimization including a move to electronic payment methods
Organizations that adopt AP automation are able to streamline their overall procure to pay (P2P) processes and marshal their resources to survive in the post-pandemic world.
Increasing Business Intelligence with Visualization
More leaders across healthcare organizations need real-time insights into their processes, payments, and invoicing data. To address this AP departments will need to improve their capabilities to serve these organizational needs.
How can health systems do this?
- C-suite leaders must implement crisis preparedness, assess their health system’s financial wellbeing, and get to know their organization at a deeper level to prepare for the future.
- Supply chain leaders must understand how their current spend equates to outcomes, and how that spend is optimized to improve cost, quality, and outcomes (CQO).
- Risk and compliance departments should assess their spending and vendors for possible fraud – especially given the rise of cyberattacks on health systems and hospitals. Cyberattacks shut hospital operations down, costing as much as $45,700 per hour of downtime reported by Becker’s.
- Clinical leaders need to arm themselves with data that helps them to evaluate opportunities for increased standardization.
Increasing AP’s digital capabilities means increased amounts of data to manage, which is both an opportunity and burden. It’s a burden due to the fact that more tools and personnel are needed to analyze and interpret the data. However, it is also an opportunity to provide insight into a health system’s spend data – insight no other department can provide such as:
- Better financial forecasting and modeling
- Processing times
- Payment terms optimizations
- P2P control effectiveness, such as use of purchase orders and supplier use optimization
- Team member performance
- Order and invoice volume
However, manually tracking the information necessary to provide that insight is far beyond the capacity of current healthcare AP departments. Adopting digitalization and tracking automation provides the flexibility today’s health systems need. Those organizations which embrace this opportunity are the ones who will thrive in the post-pandemic era.
Leveraging KPIs for Efficiency and Improvement
Increasing AP’s business intelligence and visualization not only provides insight into the financial health of an organization but also provides information to meet performance metrics and achieve leaner processes.
AP has traditionally been focused on calculating their average days-to-pay vendor invoices and managing their total volume of transactions on a monthly basis. Now departments can focus on next-level metrics and key performance indicators (KPIs) such as costs of processing a single invoice, days payable outstanding, and discounts captured.
With proper KPIs in place, AP can leverage data visualization tools, integrate real-time ERP information, and provide the flexibility to develop ad hoc reporting. This provides the necessary information in the appropriate context of departmental and organizational goals.
Strategic Vendor Management
It is important to note that AP is not responsible for all aspects of vendor management. However, it is essential they work with their procurement counterparts to build and manage a strategy. A successful strategy will lessen IRS fines, streamline data management, and decrease duplicate and other incorrect payments. Strategic vendor management is essential while health systems are tasked with doing more with fewer resources and staff.
AP serves as the primary, day-to-day contact point between the health system and its vendors. Due to this, their vendor relationships must process timely payments while also protecting the organization against errant disbursements.
Furthermore, AP must fight the fires of exceptions management, invoices received without POs, and collecting all associated account information for each transaction. AP must do the part to ensure health systems do not fall victim to a vendor-centric approach to managing their vendors, leaving the control in the hands of vendors.
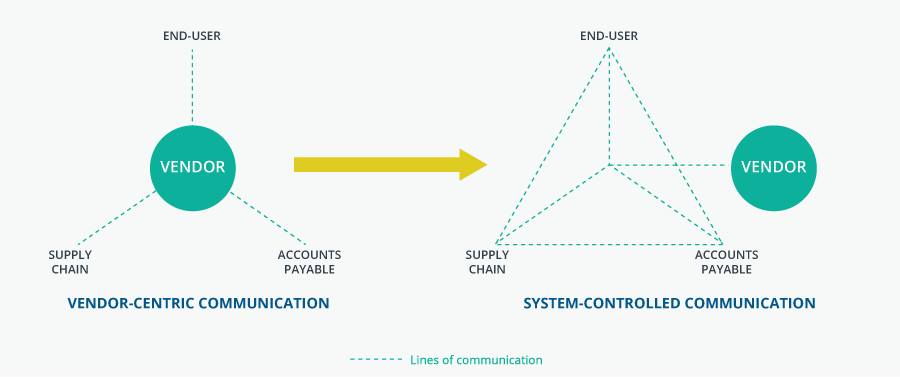
To better manage vendors, AP should take a more proactive and strategic organizational role within this process. A role that leverages all the resources of their own organization to take control back from their vendors. This means applying all the above trends throughout the P2P process. Doing this allows for increased interdepartmental communication, defined processes, accurate data capture, and guidance to the rest of the organization on how to improve.
We’re here to help consult throughout the P2P process take on the trends and challenges mentioned here. Contact us with any questions or concerns to get your AP department on the right track.
