With over 30%* of all operational expenses, purchased services can be a revealing spend category for healthcare systems. Why? Purchased services often act as a litmus test for how well an organization systematizes its operations, communicates across departments, and optimizes their resources.
Ultimately over the next decade, the health systems that fine-tune their purchased services management process will thrive, while everyone else falls behind.Purchased Services Quick Facts:
Purchased services include any and all services that are performed by a third-party vendor rather than done by the health system itself. Examples include landscaping services, credit card processing, and transcription.
![]()
Health systems across the nation spend over $300,000,000,000 per year on purchased services. A figure that is certain to go up in the coming years as organizations move toward cloud-based, digital health solutions.
All health systems require purchased services, though few have adopted a proactive and comprehensive approach to optimizing them.
Savings Opportunities with Purchased Services
According to analytics firm Conductiv, hospitals overspend by as much as $39 billion per year on purchased services alone.
While that number may seem alarming, it actually represents an opportunity for health systems willing to take on their purchased service processes and reduce overcharges. However, many system leaders hear that the industry overspends billions each year and nod their collective heads, thinking, “with what I’ve seen around here, I’m not surprised.”
Why has it become normal practice to accept billions of dollars being lost a year?
Challenges with Managing Purchased Services
Purchased services are an inherently difficult category for health systems to take control of for a number of reasons.
Organization-wide disbursement of needs
A truly comprehensive list of all purchased services your health system needs might exceed 1,000 unique services. Everything from laundry to clinical equipment maintenance to staffing solutions must be accounted for. Each of your departments has its own needs and requirements, and they must all be accounted for in your overall organizational purchased services approach. Corralling the correct information in order to make the proper decisions is a challenge in and of itself.
If not done correctly, you will overspend on these services compared to a more strategic approach.
Variations of Need
In today’s healthcare landscape, multi-entity IDNs fall in line with the status quo. Even independent, smaller hospitals are often affiliated with larger organizations in some way (clinically or financially); but with size comes challenges. Health systems with regionally diverse hospitals often have different needs – snow removal being a common example. An organization might require regular snow removal at one location and hardly any at another. Handling these variations increases the complexity of the task.
Variations like these require more of your time to create flexible frameworks and targeted approaches.
Numerous, diverse service providers
In addition to managing your internal information to determine what you need, you must also look externally to determine what is available. The range of services a health system may use can mean dealing with everyone from a local mom-and-pop restaurant to a regional or national cloud-based IT provider. These interactions will necessarily require different communications and approaches to interacting with the vendors. Your approach must be rigid enough to reduce variability but flexible enough to account for these different scales.
Your team must be comprised of professionals adept at varying communication styles.
Lack of Resources: People, Process, Tools
Many health systems are not yet at a point where they have a single source of truth for their data and analytics capabilities. Often, this resembles a patched-together network of systems that do not seamlessly integrate. Laid atop that system of tools are non-standardized processes for controlling purchased services spend, which creates too many variables to easily manage. Finally, due to the recent financial turmoil amidst the COVID-19 pandemic, health systems are unable to dedicate the proper amount of their people’s time to this area, instead opting for item-related savings – the “low-hanging fruit” that, while valuable, tends to be a moving target each year.
Getting to the point of a true single source of truth that interoperates with all accompanying systems requires strong executive visions and a multi-year organizational effort.
Intangibility of Services
A complicating factor within the purchased services space is that the services themselves are not easily identified as received or not. This conflicts with a key internal control within most ERP systems that require items or services to be “received” before payment can be processed against a purchase order (PO), leading to a backlog of invoice exceptions. Exceptions then result in missed discounts from vendors or shipping and credit holds by suppliers. Many organizations circumvent this control by not requiring POs for some or all of their purchased services to spend or by utilizing an automatic receipt on their POs. Both practices, while removing common bottlenecks within the payment process, reduce the ability to identify pricing anomalies and overcharges from vendors.
When processing payment for purchased services, it is difficult to balance speed and ease of use against a need for internal controls and compliance.
Benchmarking difficulties
Due to all of these challenges and variations, it is often difficult to make an “apples-to-apples” comparison when considering which service option is best for you. Sharing data between health systems are not common, and therefore it is difficult to gauge what other similar organizations pay for certain services. This inability to benchmark is complicated by the fact that health systems have difficulty managing the “line item” detail of their current purchased services spend. Without a proper benchmark, making improvements is next to impossible if you are struggling to accurately understand your current state.
Purchased services brings with it the challenges of imperfect information, widely disbursed, and not easily obtained.
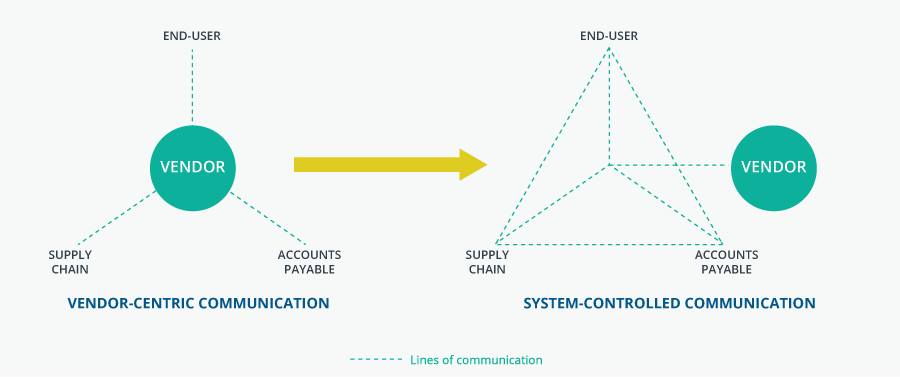
Take back control from your service vendors
Too many organizations fall into the trap of a “vendor-centric” approach to managing purchased services. This means that each department within the health system tends to deal directly with the vendor individually, rather than with each other in a strategic way. This is not only inefficient but also leaves hospitals vulnerable to services being performed that were not part of the contract or charging for services that may not have been performed at all.
The strongest organizations are proactive in taking back control from their vendors. This means increased interdepartmental communication, defined processes specific to each area of purchased services, accurate data capture, and careful contract creation and management.
TAG Inc. Vendor Communication Model
5 Tips for Managing Your Purchased Services
In order to master these challenges, here are five tips to improve your healthcare system’s strategic vision and financial sustainability within the purchased services space.
1. Use data to understand your current state
While the old adage “what gets measured gets managed” is often thrown around blindly, in this particular case it rings true. In order to improve your purchased services spend, you need to first identify what improved means. Since many organizations struggle with this most fundamental of components, you should always:
Drive as much spend as possible through your single source of truth (typically, an ERP system or other spend visualization tool).
Eliminate as many ad-hoc reports as possible from your workflows. Manually updated spreadsheets have their place, but they are error-prone and attention intensive.
Use POs as much as possible. For all recurring, fixed charges, you should utilize a proper PO process that includes the quantity and cost indicated in the contract. For all non-recurring or non-standard charges, build the Item Master to include all potential charges at their unit rate, then have end users enter a line item requisition when charges are required. This allows prices to populate as per the contract.
If you can get to the point of being able to “see the whole field,” you will identify easy wins in terms of savings opportunities.
2. Standardize Your Own Pricing
Once you have identified your current state, mine that data for opportunities to eliminate redundancies, reduce variability, and standardize pricing across your organization. Most health systems employ or are moving to a multi-entity model, whereby their organizations are comprised of various smaller hospital facilities all operating under the same corporate umbrella. In many cases, this model is the result of mergers or acquisitions that were ‘bolted on,’ which creates legacy services, pricing, and contracts in one hospital that are different from the overall parent organization.
You can immediately save money by reducing the variations that exist across different entities. However, by operating as a single buying unit, you can tap into greater purchasing power to drive better pricing across the entire health system. The result is massive, long-term savings and better overall cohesion toward organization goals.
Where possible, seek to pay a single price for the services your health system receives.
3. Use teamwork to drive value
Once you have identified your current state, mine that data for opportunities to eliminate redundancies, reduce variability, and standardize pricing across your organization. Most health systems employ or are moving to a multi-entity model, whereby their organizations are comprised of various smaller hospital facilities all operating under the same corporate umbrella. In many cases, this model is the result of mergers or acquisitions that were ‘bolted on,’ which creates legacy services, pricing, and contracts in one hospital that are different from the overall parent organization.
You can immediately save money by reducing the variations that exist across different entities. However, by operating as a single buying unit, you can tap into greater purchasing power to drive better pricing across the entire health system. The result is massive, long-term savings and better overall cohesion toward organization goals.
A cohesive, value-driven process improves quality and reduces costs.
4. Develop a process and stick to it
All too often in healthcare, processes exist in someone’s head rather than on paper. Things get done due to institutional knowledge that isn’t widely shared if it is shared at all. This creates bottlenecks, delays, and frustration from those within the process who can’t read minds – which is everyone!
If you believe your organization has a process for gathering information from end-users, identifying service vendors who fit those criteria and contracting with those vendors at market competitive rates, develop a process map that clearly puts each of those steps into a single document. This document should include named process owners, a flow of inputs and outputs from each step within the process, and examples of what happens once the process veers off the “critical path.” The exercise of putting together this in-depth document will illuminate gaps and redundancies, allowing for instant improvement.
Once complete, share the document widely with everyone who has a part in the process. Review it regularly as a department and organization as a whole. Repetition increases adherence. Over time, each review will act as a checkpoint for continued improvement.
Process mapping reduces variations and streamlines your work while also reducing frustration amongst your teams.
5. Benchmark and compare with peers
Once you understand your own spend, it is imperative to compare that spend with other organizations like your own. How do you measure up?
Utilizing resources from either a GPO, regional or national affiliation, or a specialty software tool TAG’s SpendSuite, create metrics for areas where your pricing or spend doesn’t measure up to other similar organizations. Be cognizant of the “apples-to-apples” problem by reducing services down to their smallest unit of measure whenever possible. Then take this three-step approach:
Identify all instances where your organization’s spend is not best-in-class. Those are savings opportunities.
Prioritize those savings opportunities based on your larger strategic goals and available resources.
Develop milestones for your team to close the identified process gaps and re-assess your progress until you achieve your goals.
Getting your organization as close to benchmark standards reduces your financial burden – funds that can be repurposed for improving patient care.
Given all the complexities and challenges surrounding purchased services, the task before you is not an easy one. However, the opportunity to drive big, sustainable savings to your health system is too important to pass up. It is one of the key factors that will impact how close to the leading edge your organization operates from in the next decade.
Remember that taking control of your purchased services through a system-centric communication model is key. From this mindset, you can act as one powerful organization that achieves your strategic goals.
Now, more than ever, health systems need creative solutions and visionary leadership to bolster themselves against today’s challenges and tomorrow’s unknowns.
Need help establishing or optimizing your purchased services management and payment process? Reach out now to get started.
* Information from TAG\’s 30+ years of data analysis in the healthcare industry.
