
TAG’s Mike Nisivoccia to Speak at NEHIA 2019
November 27, 2019
Process Mapping: An Essential Tool for Your Procure-to-Pay Processes
January 29, 20202020 is expected to be another year of transition for healthcare providers as systems continue to evolve through mergers and acquisitions (M&A), restructures, and strategic shifting of resources. These types of transitions affect every aspect of a health system’s business operations, including the entire Procure-to-Pay (P2P) landscape. As hospitals continually attempt to do more with less, increasing efficiencies within the financial segments of the organization is becoming more crucial than ever.
Moody’s Investor Relations reports a stable outlook for the not-for-profit and public healthcare sector, indicating further expansions through M&A’s. Coupling the M&A generated gain in negotiating power over insurers and vendors with increased financial efficiencies will provide many healthcare systems the boost they need to expand service to their patients and communities.
Five trends stand out that will help shape healthcare’s P2P process in 2020:
1. Procure-to-Pay as an Ecosystem
 An ecosystem is an interconnected network of complex systems that, when working together, benefit the whole network. Similarly, the P2P process of a healthcare system is a network of co-dependent systems that only function optimally when working in unison.
An ecosystem is an interconnected network of complex systems that, when working together, benefit the whole network. Similarly, the P2P process of a healthcare system is a network of co-dependent systems that only function optimally when working in unison.
Traditionally, the functions of the P2P process have been viewed individually – each department is responsible for only its piece of the process. Rather than working together to achieve an efficient and effective P2P process, departments blame each other for poor output and time lag, causing division and perpetuating the problem. However, forward-thinking health systems are realizing that the P2P process is essential to the well-being of their organization.
“Driving this process to function as a cohesive ecosystem requires a dynamic shift in culture, requiring leadership to view departments wholistically to reduce waste and improve the bottom line. Only when all parts of the process are functioning to benefit the whole system will the process be beneficial,” said Bruce Kellerman, PhD, Vice President of Business Development and Marketing at TAG, Inc.
2. A Focus on Risk Management
Departments involved in P2P processes must begin preparing for the unexpected by evaluating the risk associated with contract management, compliance with programs such as 340B, and devising processes to stop leaking funds. With increasing threats to the viability and security of healthcare organizations, mitigating risk at all levels is essential to both daily operations and achieving long-term goals.
In some instances, mitigating risk generates revenue or additional resources for the organization, in addition to providing much-needed safety nets. For example, by focusing on compliance within 340B, a healthcare system minimizes patient and organizational risk. This focus also allows the system to effectively utilize its 340B program, providing the system with funds to expand community outreach, meet patient needs, and achieve annual goals.
3. Strategic Vendor Management
Strategic vendor management requires all functions of the P2P process to be working optimally, providing significant returns to the system. We continually work with clients that fall victim to a vendor-centric approach to managing their vendors, leaving the control in the heads of suppliers performing the services.
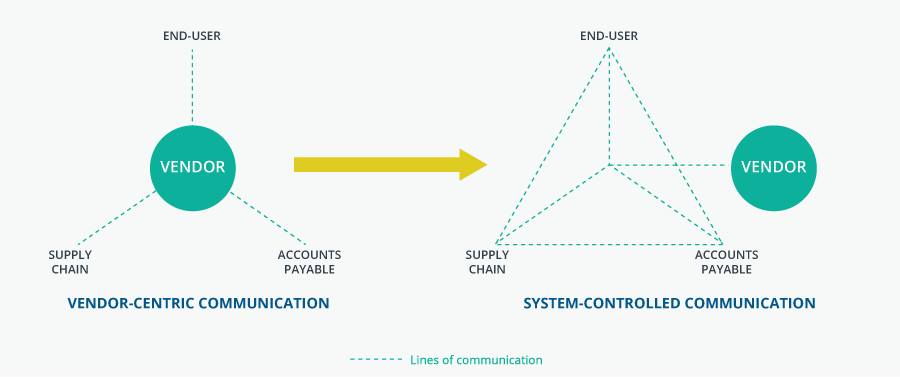
To mitigate risk associated with managing a wide range of vendors, health systems must be proactive in taking control back from their vendors. This means increased interdepartmental communication, defined processes to receiving and paying for goods/services, accurate data capture, and careful contract creation and management. The goal is to move away from a vendor-centric model to a system-centric communication model where internal departments work together before, during, and after goods or services are received to ensure vendor compliance.
4. Data Analysis to Manage Processes
As the use of data analysis within healthcare continues to expand so does its uses. In a world of constantly competing priorities, using data to identify obsolete and ineffective processes can help organizations dig beneath the surface. Oftentimes, processes seem effective on the surface but actually leave gaps and loopholes that undermine the process’ output. Addressing these concerns impacts multiple levels of the organization, making the path to a complete solution seem daunting. However, data allows all levels of an organization to understand the current state and the desired state of processes in a quantifiable way. By providing statistics and goals, processes can be transparently impacted by using data to drive organizational change.
5. Predictive Analysis with AI
Predictive analytics provide a way for health systems to use their current and historical data to create models that can predict future results. In the P2P ecosystem, predictive analysis is an important tool hospitals must adopt to reduce risk, detect fraud, and optimize operations.
Managing risk should be a priority of every entity, department, and employee at your health system using the methods mentioned above. Predictive analysis is based on AI and machine learning that develop patterns over time. For example, an AI system can learn your health system’s buying patterns to determine procurement schedules and buyers. With the correct controls in place, administrators can be alerted to anomalies that, when investigated, may lead to fraudulent activities.
Leaders in your health system’s P2P space are faced with allocating resources that are limited based on the needs of your organization. However, leaders are tasked with finding ways to improve efficiency to make the most out of the resources they have without disruption to their current workflow. By modeling the existing P2P processes and utilizing predictive analysis, leaders can determine the impact that a change may have on the process without putting resources at risk.
Does our healthcare system have a plan for 2020 to address these trends? To stay competitive, your P2P teams need to be able to adapt to new technology and processes while leaders need to focus on a culture change widening the scope of the “P2P team.”
We can help healthcare’s CFOs and Supply Chain Leaders to give their health system a competitive advantage by staying on top of these trends. What to learn how? Send us a message now.

